- Eyes feeling dry, sore, or irritated
- Tearing or buildup of particles in the eyes
- Sensation of itchiness, grittiness, or eye strain
- There may be light sensitivity, e.g. after prolonged screen use
Article Sections:
What is Dry Eye Disease (DED)?
1. Aqueous Deficient Dry Eyes (ADDE)
2. Evaporative Dry Eyes (EDE)
Things like air pollution, poor quality or unclean cosmetics, hormonal changes, surgery, stress, and anxiety may increase vulnerability to dry eye symptoms and disease.
Ocular allergies and systemic disease as well as smartphone use were found to be associated with DED in youths (See Stapleton et al., 2024)
Some drugs may cause dry eye, for example several anti-histamines (Penn Medicine, 2025).
What can we do?
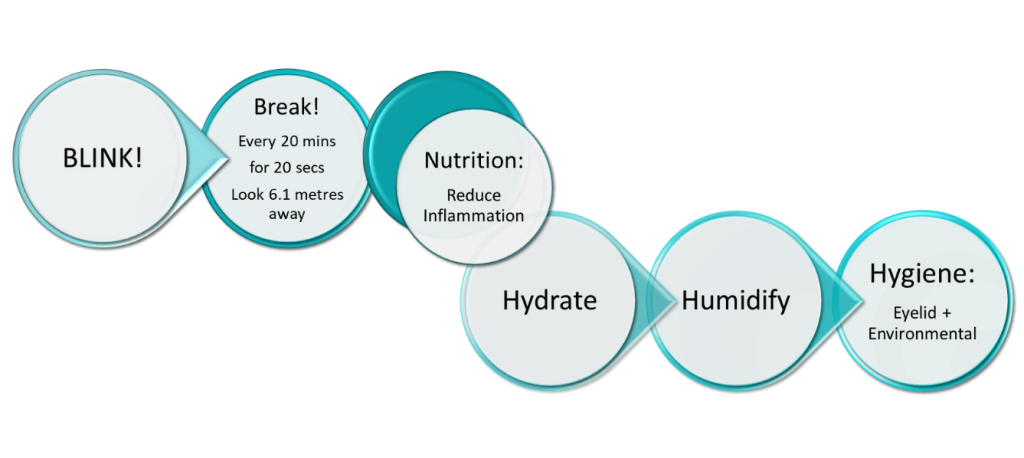
BLINK! More Frequently
Break! Follow the 20-20-6.1 Rule
Nutrition: (e.g. Include Omega-3s and Antioxidants in Your Diet)
Hydrate! Drink enough water
Humidify! Get outdoors more or use a humidifier
Hygiene: Eyelids and Environmental
What can we use?
Artificial Tears
Gel Drops or Ointments
Preservative-Free Drops
Medicated Eyedrops
Another Route: Meibomian Gland Stimulation
What to expect
- Sessions last approximately 20 minutes per eye.
- Most patients undergo four treatments over 4 weeks.
- No anaesthesia or recovery time is required, patients can resume normal activities immediately.

Key benefits
- Improved gland function leading to a more robust oily layer in the tear film
- Reduced tear evaporation and longer-lasting relief from dryness
- Fewer symptoms of burning, irritation, and redness
- Enhanced comfort during extended screen use and in dry environments
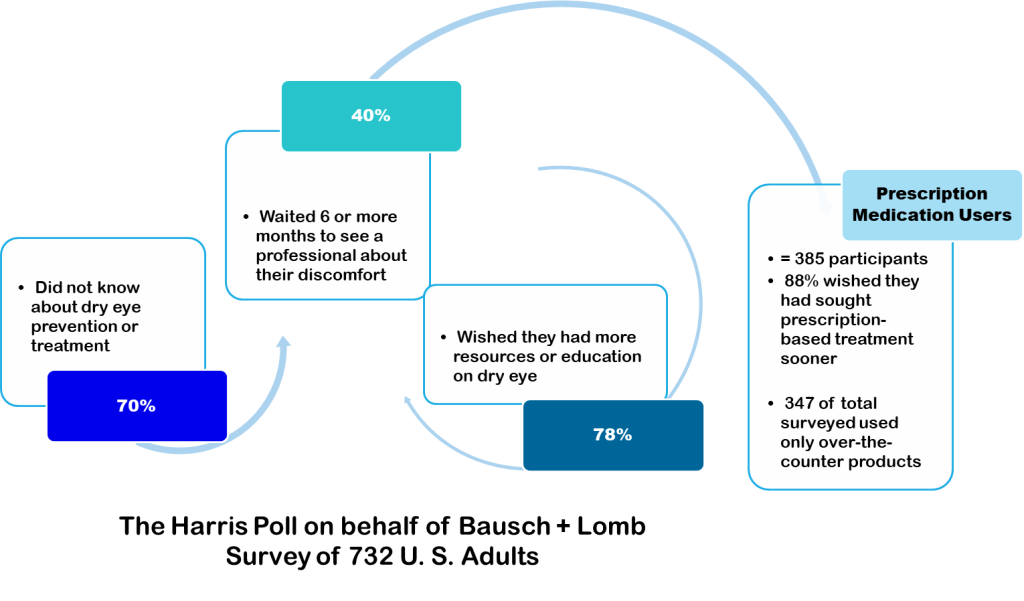
- 1 Report and Campaign Announcement : https://www.bausch.com/newsroom/news/?id=276 Bonavitacola, J. (2025, July 8). Education Surrounding Dry Eye a Persistent Barrier in Treatment. AJMC. https://www.ajmc.com/view/education-surrounding-dry-eye-a-persistent-barrier-in-treatment Bonavitacola, J. (2025, July 8). Dry Eye Awareness Month Highlights Condition Affecting Millions. AJMC. https://www.ajmc.com/view/dry-eye-awareness-month-highlights-condition-affecting-millions
- 2 According to material prepared by Bausch + Lomb (2025), Dry eye can hide in plain sight. Link: https://www.bausch.com/siteassets/pdf/dry-eye-can-hide-in-plain-sight.pdf See also Stapleton, F., Velez, F. G., Lau, C., & Wolffsohn, J. S. (2024). Dry eye disease in the young: A narrative review. The ocular surface, 31, 11-20. https://doi.org/10.1016/j.jtos.2023.12.001
- 3 Craig, J. P., Nichols, K. K., Akpek, E. K., et al. (2017). TFOS DEWS II Definition and Classification Report. The Ocular Surface, 15(3), 276–283. https://doi.org/10.1016/j.jtos.2017.05.008
- 4 Varacallo, P. (2025, July 1). Here’s How You Know You Have Dry Eye: Expert Doctors on the Confusing Symptoms, Causes, and the #1 Mistake Patients Make. The Healthy. https://www.thehealthy.com/eye-care/what-to-know-about-dry-eye-expert-doctor
- 5 Bu, J., Liu, Y., Zhang, R., Lin, S., Zhuang, J., Sun, L., Zhang, L., He, H., Zong, R., Wu, Y., & Li, W. (2024). Potential New Target for Dry Eye Disease—Oxidative Stress. Antioxidants, 13(4), 422. https://doi.org/10.3390/antiox13040422
- 6 Kangari, H., Eftekhari, M. H., Sardari, S., et al. (2013). Short-term Consumption of Oral Omega-3 and Dry Eye Syndrome. Ophthalmology, 120(11), 2191–2196. https://doi.org/10.1016/j.ophtha.2013.04.006
- 7 Epitropoulos, A. T., Donnenfeld, E. D., Shah, Z. A., Holland, E. J., Gross, M., Faulkner, W. J., Matossian, C., Lane, S. S., Toyos, M., Bucci, F. A. Jr., & Perry, H. D. (2016). Effect of Oral Re-esterified Omega-3 Nutritional Supplementation on Dry Eyes. Cornea, 35(9), 1185–1191. https://doi.org/10.1097/ICO.0000000000000940
- 8 Markoulli, M., Ahmad, S., Arcot, J., Arita, R., Benitez-del-Castillo, J., Caffery, B. et al. (2023). TFOS Lifestyle: Impact of nutrition on the ocular surface. Ocul Surf, 29, pp. 226-271. https://doi.org/10.1016/j.jtos.2023.04.003
- 9 Patel, S., Marshall, J., & Fitzke, F. W. (2015). Hydration, fluid regulation and the eye: In health and disease. Clinical & Experimental Ophthalmology, 43(10), 915–924. https://doi.org/10.1111/ceo.12546
- 10 Nguyen, L., Magno, M.S., Utheim, T.P., Jansonius, N.M., Hammond, C.J. & Vehof, J. (2023) The relationship between habitual water intake and dry eye disease. Acta Ophthalmologica, 101, 65–73. https://doi.org/10.1111/aos.15227
- 11 Nguyen, L., Magno, M.S., Utheim, T.P., Jansonius, N.M., Hammond, C.J. & Vehof, J. (2023) The relationship between habitual water intake and dry eye disease. Acta Ophthalmologica, 101, 65–73. https://doi.org/10.1111/aos.15227
- 12 Nguyen, L., Magno, M.S., Utheim, T.P., Jansonius, N.M., Hammond, C.J. & Vehof, J. (2023) The relationship between habitual water intake and dry eye disease. Acta Ophthalmologica, 101, 65–73. https://doi.org/10.1111/aos.15227
- 13 Nguyen, L., Magno, M.S., Utheim, T.P., Jansonius, N.M., Hammond, C.J. & Vehof, J. (2023) The relationship between habitual water intake and dry eye disease. Acta Ophthalmologica, 101, 65–73. https://doi.org/10.1111/aos.15227
- 14 Liu, Z., Xie, Y., Zhang, M., & Pflugfelder, S. C. (2000). [Zhonghua yan ke za zhi] Chinese journal of ophthalmology, 36(2), 131–134. https://pubmed.ncbi.nlm.nih.gov/11853602
- 15 Agarwal, P., Craig, J. P., & Rupenthal, I. D. (2021). Formulation Considerations for the Management of Dry Eye Disease. Pharmaceutics, 13(2), 207. https://doi.org/10.3390/pharmaceutics13020207
- 16 Baudouin, C., de la Maza, M. S., Amrane, M., Garrigue, J.-S., Ismail, D., Figueiredo, F. C., & Leonardi, A. (2017). One-year efficacy and safety of 0.1% cyclosporine A cationic emulsion in the treatment of severe dry eye disease. European Journal of Ophthalmology, 27(6), 678–685. https://doi.org/10.5301/ejo.5001002