Adults (18 to Senior)
In the context of eyecare, adults are typically divided into two age groups with seniors (>60) as a subset of those aged 40 and above
Primary eyecare is a crucial component of health. Several eye diseases are age-related and some can lead to irreversible loss of vision. To protect their sight, it is important for adults and the elderly to schedule regular appointments with a primary eyecare practitioner so that conditions like glaucoma and diabetic retinopathy can be detected and managed early using specialised imaging equipment. For example, in 2020, SNEC data showed that glaucoma accounted for 34% of blindness cases in Singapore, with a more recent (2022) estimate of 10% of the population affected.
Patients and their families should be aware that most sight loss is preventable if detection and intervention is early.
It is estimated that 80% of vision loss and blindness can be prevented or treated (IAPB, 2024)
Acting to protect our eyes also preserves quality of life and mobility for extra years as we age.
Most people with visual impairment and blindness are over 50 years old (WHO, 2023)
Glaucoma can be controlled and irreversible vision loss can be prevented if it is detected early. There are usually no warning signs or symptoms.
Up to 50% of cases in Singapore might be undiagnosed. Governmental efforts to increase screening accessibility and frequency have improved early detection and glaucoma patient outcomes.
Diabetic Retinopathy can eventually affect all patients with diabetes and has no symptoms at early disease stages. Lack of awareness, detection, and early intervention means this is a leading cause of blindness for working age Singaporeans (SNEC, 2020)
Fundus imaging of blood vessels in checks for retinopathy can serve as an additional way to monitor and evaluate diabetes management programmes. This is done in collaboration with a patient’s doctor or diabetes specialist.
18 – 40 years old
Singapore’s adult population aged 18 to 40 years old is typically affected by myopia, with incidence of dry eye disease, digital eye strain or computer vision syndrome, and occasional injuries. Eyecare is more routine for this group. It is good to keep informed and ask your optometrist about sight-protective lifestyle habits, including contact lens care and digital & solar hygiene.
Also be aware of any family history of eye disease, be conscious of how to manage refractive errors, and exercise caution about products and environments that may be adversely affecting your eyes’ surface or safety.
40 and above
In the above 40 age group, risk of eye disease and complications naturally rise with age, which is why sticking to a check-up schedule is so important for adults and seniors.
Seniors (aged 60 and above) as a subgroup may require more frequent checks to manage ongoing conditions.
- An earlier diagnosis and intervention means better outcomes and lower impact of ocular pathology.
- Early intervention means more vision can be preserved, and that disruption to quality of life and finances is minimised
- Comprehensive eye examinations done with special equipment by a qualified practitioner are required annually because several eye diseases manifest in symptoms for the patient only when it is ‘too late’, after cellular, nerve, or tissue damage has occurred.
- Proper eyecare and protective habits in childhood, adolescence, and adulthood translates to fewer risks at advanced ages.
- Seniors may require moral and physical support to make it to their appointments. Adult children play a crucial role in getting their aged relatives to a check-up.
Family visits are common and very welcome at Stan Isaacs
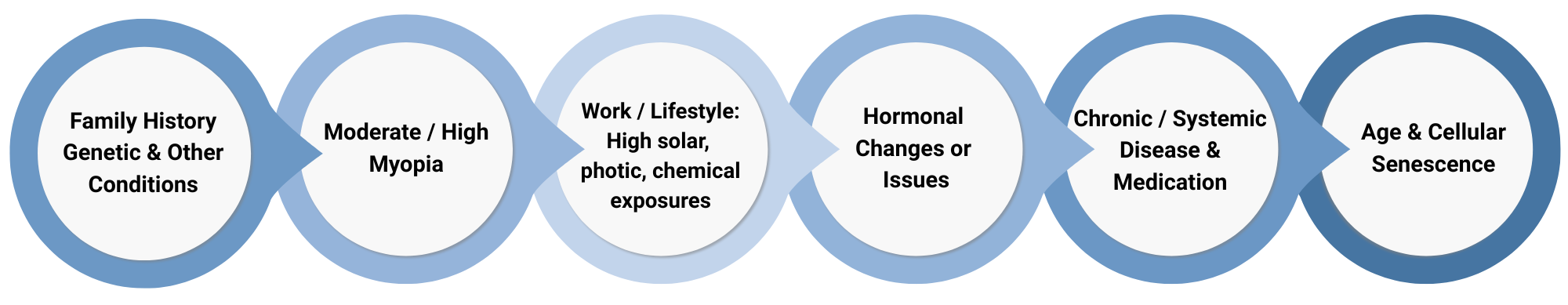
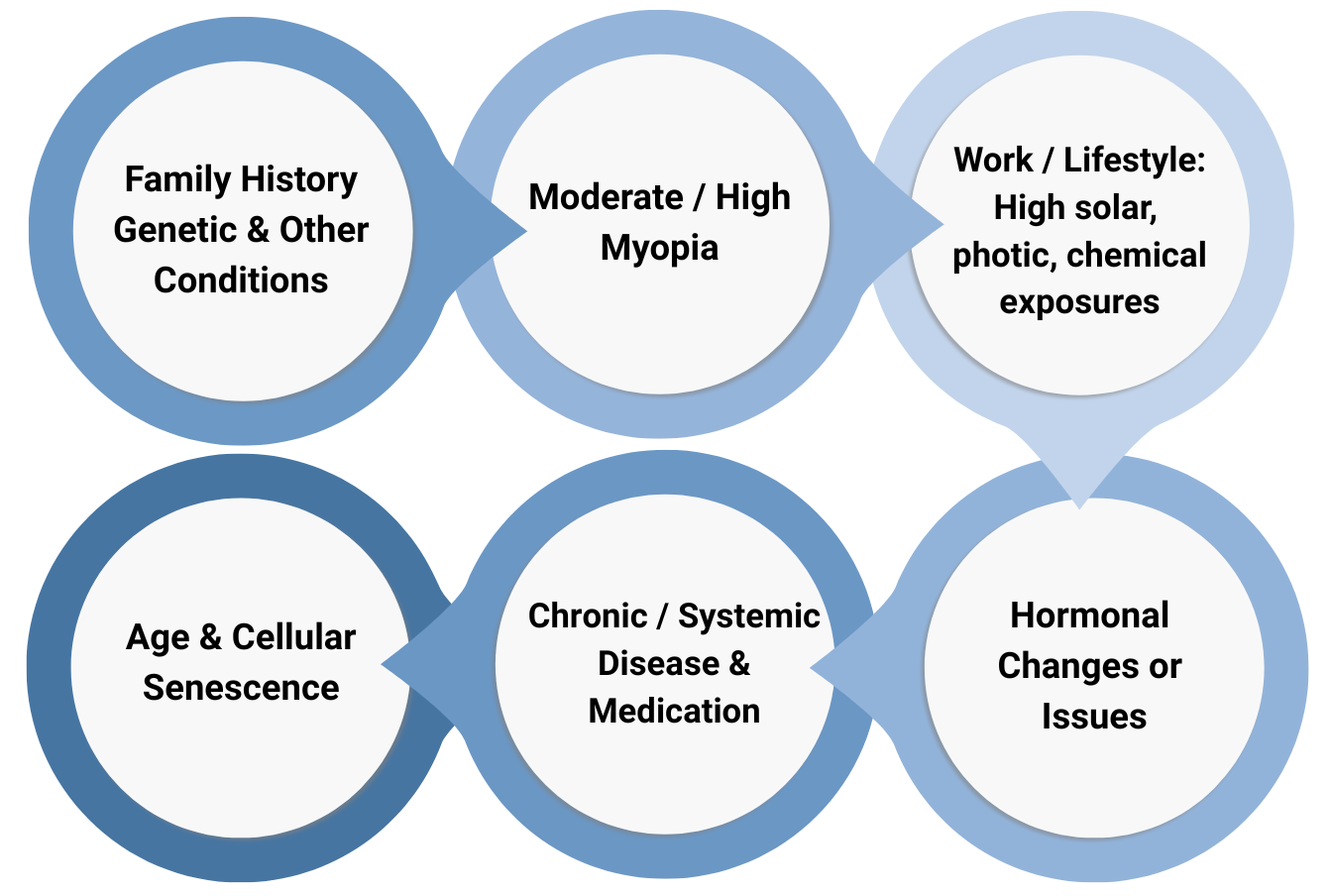
Around the age of 40, the muscles in human eyes start to lose elasticity, so presbyopia becomes an issue which requires special glasses or lenses for close-work tasks. Cataracts and glaucoma risks start to rise at around the age of 45. Risk of these conditions and myopic macular degeneration are higher if the patient has moderate or high myopia.
Chronic and systemic conditions further raise risks for ageing eyes, and serve as additional risk factors for several types of age-related eye diseases.
Certain medications (e.g. steroids, selective seronotonin reuptake inhibitors, non-steroid anti-inflammatories), treatment protocols, and hormonal conditions may also affect vision. This is best disclosed during an eyecare appointment for proper diagnosis and management.
General Risk Factors for Adult Eye Diseases
Please feel free to contact us if you have any problems or questions.
We are happy to assist over the phone, by email, or to schedule an appointment if necessary.
Check-up Schedule
We recommend that adults attend a check-up every six months unless otherwise recommended by their optometrist, ophthalmologist, or other medical professional. Ongoing conditions, a family history of glaucoma and macular degeneration, or pre-existing systemic conditions such as diabetes and hypertension may indicate higher risk and a requirement for more frequent eye checks, e.g. every 3 months.
An appointment could take approximately 30 – 45 mins, depending on your unique condition.
Tests
Comprehensive eye examinations are designed to detect onset of various ocular pathologies before there is permanent cell damage or vision loss, to update prescriptions (e.g. for presbyopia), and to make sure nothing else is remiss.
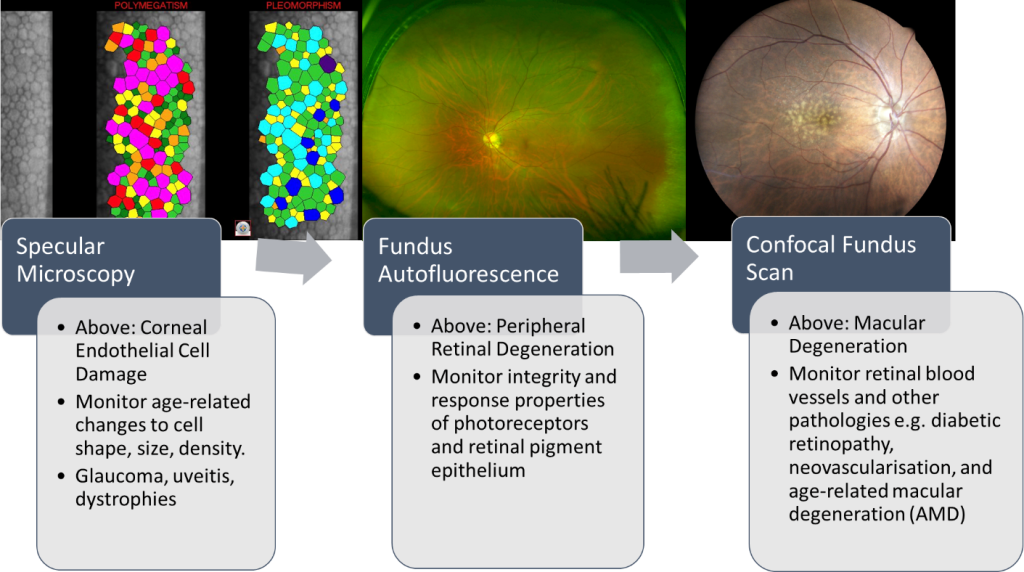
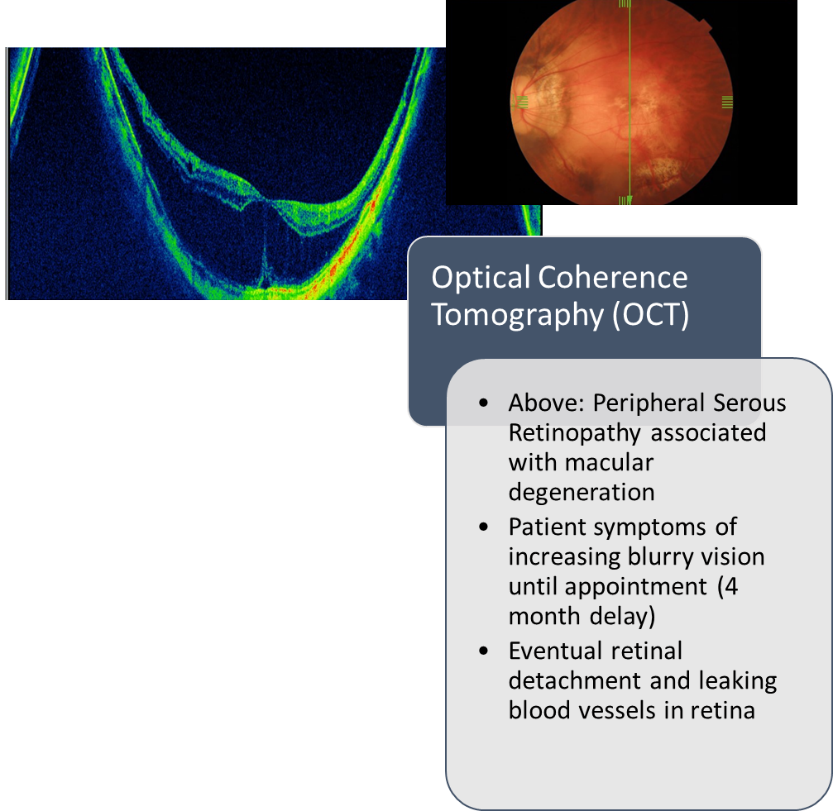
Over the past few years, there have been significant technological advances in ocular imaging. Some equipment is able to measure changes in tissue at the micrometer scale, while others can be employed to count cell types, density, and health in the retina. Regularly attending eyecare appointments with specialised diagnostics instead of waiting for a problem or emergency to manifest is the best approach to protecting lifelong sight.
What we look out for:
18 & up
Common conditions for our patients in this age bracket include:
- Myopia, including adult-onset
- Ongoing monitoring of other Refractive Errors
- Dry Eye Disease (DED)
- Eye Strain & Computer Vision Syndrome (CVS)
- Eye Infections / Allergies
- Eye Injuries (activity & myopia-related)
40 & up
Common conditions for our patients in this age bracket include:
- Presbyopia
- Night blindness and trouble with glare
- Glaucoma
- Cataracts
- Dry Eye Disease (Gland-related)
- Age-related Macular Degeneration (AMD)
- Eyelid Disorders
- Eye Injury (Vulnerability)
- Complaints of spots, floaters, or flashes
- Diabetic & Hypertensive Eye Diseases
Lifestyle Habits
Aside from keeping to your annual or recommended appointment schedule, there are several things you can do to maintain healthy eyes as an adult.
Near Work Habits
- A popular one to prevent eye strain is the 20-20-20 rule: For every 20 minutes of work, stare at an object at least 20 feet (6 meters) away for at least 20 seconds.
- People also tend to blink less when on a computer, contributing to eye dryness. Try to be aware and consciously increase your blink rate.
- During breaks, try to add following distant moving objects with your eyes, letting your gaze roam freely, to relax instead of focus, or stare at natural greenery and scenery.
- Try not to read in dark surroundings. Increase the visual contrast of text and keep good posture, with close work objects at or around eye level, at arm’s length.
Digital hygiene
- Limit prolonged and night time exposure to LEDs and other bright artificial lights.
- Minimise screen glare and direct exposure to bright artificial lights.
- This helps with sleep and improving night-time melatonin production. Melatonin can act as an antiantioxidant agent for mitochondrial and neural health.
- Take breaks and be sure to blink when doing close work on computers or other devices.
- Do not aim to permanently block all blue and violet light bandwidths.
- Watch your posture, and try to keep screens and reading material at just below eye- height.
- Many children’s myopia apps now have alerts for posture, reading distance, and nearwork breaks.
Solar hygiene
- Get natural sunlight exposure especially at dawn and dusk to help set your internal body clock, with includes a circadian rhythm for ocular cells based on several components of the visible and non-visual light spectrum.
- Set a limit for exposure to bright UV-rich sunlight and glare, e.g. off snow and white surfaces. Stay in the shade or use hats and UV-blocking sunglasses when appropriate.
Contact Lens and Spectacle Care
- Be sure to follow instructions
- Replace or fix visual devices and equipment as soon as there is a problem
- Call and see your primary eyecare practitioner if you experience itching, redness, or other problems after changing eye drop or solution brands.
- Never buy from unregulated platforms or use counterfeit products on your eyes.
Use of Beauty Products
- Certain chemicals and compounds can act as irritants or yield allergic reactions
- Makeup if improperly applied or removed can be associated with dry eye disease, or lead to blockages and scratches on the eye.
- NEVER EVER apply non-medical grade products directly to your eye surface.
- Aim to always use clean, high quality products when it comes to your eyes. Be highly sceptical of internet and aesthetic trends e.g. scleral whitening.
- Talk to your optometrist about proper use of cosmetic and other coloured contact lenses.
Nutrition
- A healthy diet which limits incidence of hypertension and diabetes is beneficial for the eyes, and part of managing age-related complications.
- Eat Visually: Vary your intake by going for natural and beautiful colour variations in your proteins, fruits, and vegetables. This is a neat and easy way of including a wide assortment of vitamins and antioxidants.
- There is indirect evidence but a general understanding that a nutrient-rich diet with limits to processed food, simple carbohydrates, and sugar intake can be one way to improve general health and reduce the risk of certain ocular diseases, e.g. dry eye, photoreceptor degeneration.
- Intake of healthy fats improves tear film quality, gland function, and ocular surface lubrication, reducing incidence of dry eye.
- Supplements like the AREDS2 formula may be recommended for macular degeneration in collaboration with your doctor.
Physical Fitness and Engagement
- Keeping fit and active improves general health, mental and neural health, and blood circulation.
- Delicate cells and tissue in the retina are nourished by blood supplied through the tiny vessels of the choroid, so it is important to keep things flowing smoothly.
- One of the first effects of sight loss conditions is a reduction in confidence, mobility, social engagement, and physical activity. Therapeutic approaches for these individuals show greatest success when paired to a sense of physical agency and social inclusion.
- * Glaucoma patients need to be cautious about certain exercises and intensities that affect intraocular pressure
Special Risks for Adult Myopes
Due to scleral remodelling and damage to posterior ocular tissue as a result of eyeball elongation, having moderate or high myopia increases the risks for several age-related eye diseases. This is why it is so important to control progression at younger ages and early stages.
For all ages, having highly myopic eyes and more fragile tissues at the posterior surface increases the chance of a retinal detachment, which is a medical emergency requiring quick surgery to prevent sight loss.
Age and moderate myopia interact to increase the risk of several ocular diseases. Past the age of 45, having myopia seems to increase the risk of cataracts, glaucoma, and macular degeneration. According to a review and meta-analysis by Haarman et al. (2020), the odds ratio for open-angle glaucoma increases to 2.92 at moderate and high levels of myopia. In the case of myopia macular degeneration, the odds ratio for high myopes is 845 versus 72.7 for moderate myopes. Complications as a result of myopia make it one of the leading underlying causes for vision loss and blindness in older cohorts.
| Myopia : Odds Ratio | Retinal Detachment | Glaucoma Open-angle (OAG) | Myopic Macular Degeneration (MMD) | Nuclear Cataract |
|---|---|---|---|---|
| Low | 3.15 | 1.59 | 13.57 | 1.79 |
| Moderate | 8.74 | 2.92 | 72.74 | 2.39 |
| High | 12.6 | 2.92 | 845 | 2.87 |
Compiled from data in Haarman et al. (2020)
Parents and myopic patients need to be aware of the risks for eye health in later life, and try to address the various risks of myopia progression and axial elongation. The small things we do now can make a big difference later.
Find out more about Common and Rare Adult Ocular Disorders here:
May lead to irreversible vision loss:
References
- Abdulhussein, D. & Hussein, M. A. (2023) WHO Vision 2020: Have We Done It?. Ophthalmic Epidemiology, 30(4), 331-339, DOI: 10.1080/09286586.2022.2127784
- Boyd, K. https://www.aao.org/eye-health/diseases/what-is-glaucoma
- Chay, J., Tang, R.W.C., Tan, TE. et al. (2023). The economic burden of inherited retinal disease in Singapore: a prevalence-based cost-of-illness study. Eye, 37, 3827–3833 (2023). https://doi.org/10.1038/s41433-023-02624-7
- DeBenedette, V. (2019, September 30). Vision problems? Check your medications. All About Vision. https://www.allaboutvision.com/eye-care/medication-side-effects/
- Diet and Nutrition (2023, American Academy of Ophthalmology)
- Green, M.B. and Duker, J.S. (2023). Adverse Ocular Effects of Systemic Medications. Life, 13, 660. https://doi.org/10.3390/life13030660
- Haarman, A. E. G., Enthoven, C. A., Tideman, J. W. L., Tedja, M. S., Verhoeven, V. J. M., & Klaver, C. C. W. (2020). The Complications of Myopia: A Review and Meta-Analysis. Investigative ophthalmology & visual science, 61(4), 49. https://doi.org/10.1167/iovs.61.4.49
- Relationship between dry eye disease and high myopia in teenagers investigated in study (ophthalmologytimes.com)
- Singapore National Eye Centre. (2020). Understand more about glaucoma. https://www.snec.com.sg/patient-care/conditionstreatments/eye-conditions-brochures/Documents/EN_Glaucoma.pdf
- Soh, G. (2022, October 11). AI to help detect glaucoma early among research projects to be funded under $25m programme. The Straits Times. https://www.straitstimes.com/singapore/health/ai-to-help-detect-glaucoma-early-among-research-projects-to-be-funded-under-25m-programme
- Vimont, C. (2023, April 7). 36 Fabulous Foods to Boost Eye Health. American Academy of Ophthalmology. https://www.aao.org/eye-health/tips-prevention/fabulous-foods-your-eyes
- World Health Organisation : Blindness Infographics.